Psychosis Outpatient Treatment
From Impossible to Possible: A Breakthrough in Treatment
Written by: Marie Chesaniuk, PhD
Schizophrenia Spectrum Disorders: What are they?
Schizophrenia spectrum disorders (SSDs) is an umbrella term that refers to schizophrenia and other psychotic disorders including brief psychotic disorder, delusional disorder, schizoaffective disorder, and schizophreniform disorder. These conditions have some similarities and some differences. Notably, they all share characteristic symptoms of psychosis like hallucinations, delusions, and disorganized thoughts and behavior. They diverge with respect to levels of severity, length of psychotic episodes and periods between episodes, and whether mood disorders play a role.
While SSDs (specifically during periods of active psychotic episodes and other positive symptoms) carry an increased risk of hospitalization, they can often be treated in an outpatient setting, as well.
Schizophrenia Spectrum Disorders: How are they treated? EBTs
Evidence based treatment of SSDs involves pharmacological treatment using antipsychotic medications. The efficacy of antipsychotics at improving psychotic symptoms, preventing relapse into future psychotic episodes, and even increasing life expectancy of people with SSD has been well documented. However, medication alone does not produce clinical and social improvements related to cognitive performance, social skills, quality of life, finding and maintaining a job or having meaningful personal relationships. More importantly, people with SSD themselves do not consider themselves to have achieved full recovery without these clinical and social outcomes.
There are a number of evidence based psychosocial treatments for SSDs. The table below summarizes these and what they help with, although we will focus on psychotherapeutic approaches in this article. Note that some of the psychosocial approaches to treatment listed below have also been shown to improve symptoms of SSDs in addition to improving clinical and social outcomes.
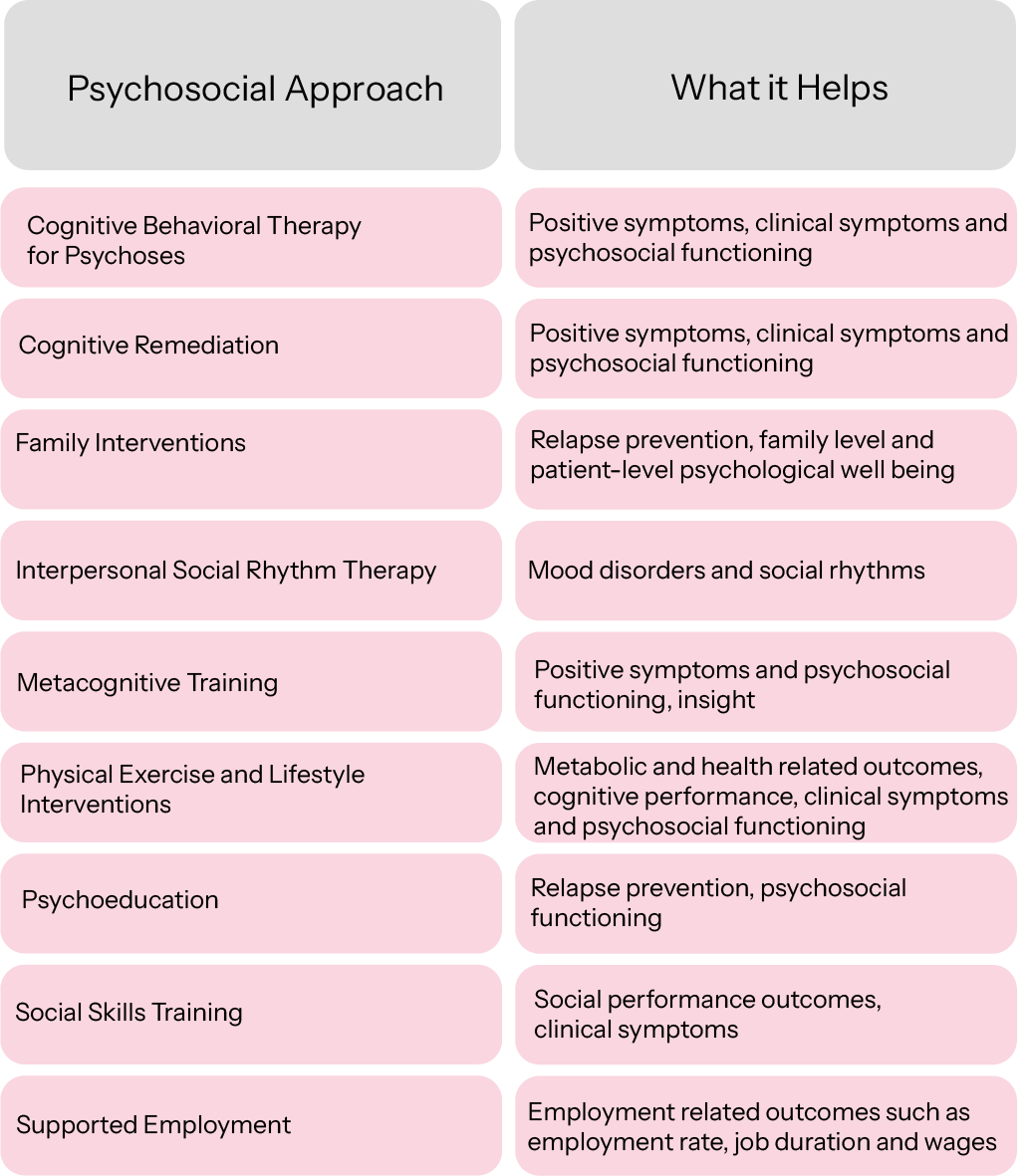
Note: This table summarizes interventions listed in a review and includes an evidence based treatment for mood disorders (i.e., IPSRT) that is in the early stages of being applied to SSDs which was not included in that review. For more detail, please see review here and IPSRT research here.
Cognitive remediation is the first line approach for individuals with lower cognitive functioning, whose cognitive functioning needs improvement before they are able to benefit from therapy. For those able to benefit from therapy, the right team makes it all possible.
Team Approach
How do you put together the best team? For successful outpatient treatment of SSDs, a team typically includes a psychiatrist, psychotherapist, and family members/caregivers apart from the client themselves. The team is nothing without good communication and treatment coordination. Weekly meetings best position team members to be able to respond quickly to urgent situations, crises, and emergencies. Regularly scheduled meetings help coordinate team members and keep everyone on the same page with respect to treatment and the wellbeing of the client.
In addition to these core team members, additional resources often tapped as part of treatment include independent living support workers, intensive outpatient program access, disability support programs, job training and supported employment and volunteer programs, transportation (e.g., PACE bus) and housing support, and crisis support lines. Additionally, independent living skills related to navigating 311 numbers for local information and guidance as well as scripts for interacting with law enforcement promote a smoother and more sustainable experience with people’s ability to live independently and receive effective outpatient support for SSDs.
The goal of outpatient treatment of SSDs is generally to minimize hospitalizations and maximize relapse prevention and wellbeing. Psychiatrists contribute to medical treatment of SSDs and any co-occurring psychiatric conditions. Those willing to provide injections can simplify medical self-management regimens by reducing the potential for missed doses, which in turn prevents relapse due to missed doses. Family members may participate in family interventions since certain family dynamics can be protective and help prevent relapse or pose an increased risk for relapse.
Cognitive Behavioral Therapy for Psychoses (CBTp) is typically an individual outpatient therapy for the client which commonly includes elements of psychoeduction, social skills training, and challenging unhelpful thoughts (e.g., reducing stigma) and learning to track and monitor delusions and hallucinations. CBTp also commonly involves behavioral activation, which helps support engagement with independent activities of daily living and social connections.
Similarly, Interpersonal Social Rhythm Therapy incorporates behavioral activation and routines with the added goal of better regulating circadian rhythms and maintaining stable and supportive social connections. The interpersonal component focuses on developing the client’s social skills and ability to communicate, handle conflict, and minimize stress and disruption due to interpersonal difficulties. These individual and family therapies help the client achieve the psychosocial recovery they hope for beyond reducing psychotic symptoms and medication management. Additionally, they position the client to better be able to maintain jobs and volunteer positions that achieve further client goals.
Red Flags and Contingency Plans
Even the best plans with the best teams and support systems cannot prevent all relapses and emergencies. It is critical to know what signs indicate cause for concern with a client. Some items to keep in mind, like sleep disruption, missed appointments, and major life stressors. Risk to self or others, co-occurring conditions that might require a higher level of care, severe side effects of anti-psychotic medications (e.g., tardive dyskinesia), severity of psychotic episode, and inability to perform independent activities of daily living all figure in decisions related to higher levels of care. Having a good contingency plan before problems arise helps everyone respond quickly and cooperatively. Agreeing in advance on what indicates need for a higher level of care and hospitalization helps everyone weather this challenge as comfortably as possible and, ideally, results in shorter and more effective hospitalizations with client and treatment team consultation and collaboration.
We can do hard things, and get through hard things, better together as a team. Outpatient treatment of SSDs is possible, desired, and part of a full and holistic recovery.
About Us
Learn moreOur Care
Learn moreWhat We Treat
Learn more